Annexes of Survivorship and rehabilitation chapter
These are the Annexes of Cancon Guide Survivorship and rehabilitation chapter.
See the full Guide and other chapters as pdf's.
Cancon Guide is the main delivery of the joint action.
Annex 7.1 Results of the survivorship care plan survey
Annex 7.2 Assessment of patient’s symptoms and needs and the orientation to adequate intervention in psychological supportive care
Annex 7.1. Results of the survivorship care plan survey
Details on data collected
A total of 21 completed questionnaires have been collected. Fig. 7A.1 shows the origins of the data by category and by country.
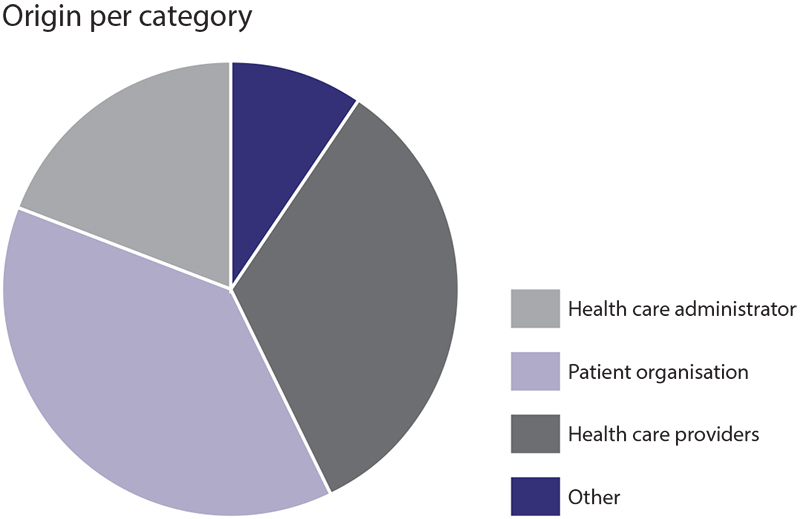
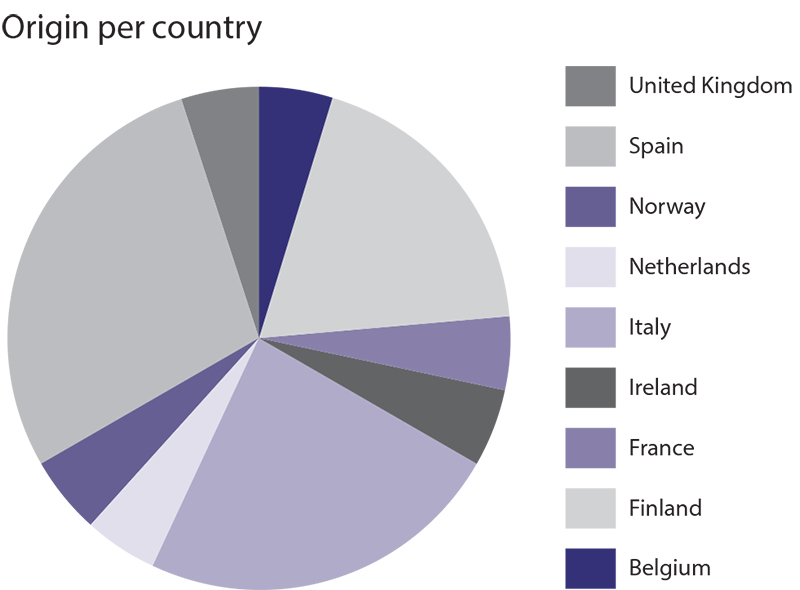
Fig. 7A.1 Data collection
Summary of results
Answers varied a lot regarding how patient follow-up is organized and implemented in the EU countries and answers can differ even within the same country. However, all respondents agreed on what is the beginning of the follow-up period: being the period after the acute treatment phase. The length of this period depends on the type of cancer and on the treatment received, for example in Belgium this period lasts for five years and can be up to 10 years in Spain.
According to the results of the survey regarding the role of care providers, the oncologist remains the leader of follow-up care after completion of the treatment. Then in most countries the GP is usually responsible for monitoring the impact of cancer and its treatment on the patient’s general health (comorbidities). The role of nurses differed a lot depending on the country, for example care coordinator in Belgium, in France and the United Kingdom, whereas the nurse may just be a contact point in Finland.
During the follow-up period, the identity of the patients, their ages and a record of the treatment(s) received are usually the minimum set of information available to care providers in all countries. In some countries, side-effect information is available (Finland, France Italy, the Netherlands, Spain) as well as rehabilitation care (the Netherlands) or medical history (Finland and Spain).
In the majority of countries involved in the survey, supportive care is provided as part of the follow-up, except in Norway and Ireland, and variable in the United Kingdom and Spain. According to the results, pain management and psychological support for patients and their relatives against anxiety and depression are the common grounds for supportive care in EU countries.
In addition to these services, symptom and late-effect management, sexuality and fertility support, as well as other supportive care such as nutrition, weight management and beauty care, are offered in a wide range of countries (Belgium, Finland, France, the Netherlands, Spain).
Regarding social support and professional rehabilitation, the situation in EU countries is more heterogeneous; only France, Finland and the Netherlands provide services such as social needs evaluation, working ability evaluation and contact details of professionals in this area. In Finland and Spain, these services are only available if the patients ask for them.
The majority of the countries that took part in the survey (76%) claimed that there was no formal survivorship care plan, apart from France, the Netherlands and Finland (only for breast cancer). For patient follow-up, countries often used a mix of tools (paper documents, oral consultations and electronic files) that were commonly shared between all professionals involved with the patient. Only Finland used a nationwide electronic system.
However, 19 respondents out of 21 (two did not answer) thought that a survivorship care plan would be an efficient tool to organize follow-up care. A survivorship care plan, according to respondents, could potentially be an important communication tool between professionals and patients to manage and structure a global follow-up taking into account all aspects of survivorship care.
In addition, 18 respondents out of 21 (two did not answer and one responded “No”) thought that a survivorship care plan would be an efficient way to improve quality of care. Not only would it improve the quality of care but it would also improve the access and continuity of care for patients.
Similarly, 18 respondents out of 21 (two did not answer and one responded “No”) thought that a survivorship care plan would be an efficient way to better involve PCPs during this period.
Participants to this survey said that there is often no coordination protocol between specialized care and PCPs. In terms of perceived barriers, the financial one came first (13 respondents), then the technical (9 respondents) and then the professional-related one (8 respondents).
Annex 7.2 Assessment of patient’s symptoms and needs and the orientation to adequate intervention in psychological supportive care
The literature review showed that early and systematic detection of needs in psychological support, social rehabilitation (in particular for return-to-work issues), physical rehabilitation, supportive and palliative care is necessary in order to orientate patients towards tailored health care interventions.
It also demonstrated the necessity to anticipate certain issues that the patients and their relatives will face during the survivorship and rehabilitation period.
In this context, one of the objectives of Chapter 7 was to set the basis of a common European process that would enable the assessment of patients’ symptoms and needs in order to facilitate their guidance towards tailored interventions in supportive care. The process is presented via several questions that reveal the modalities of implementation.
Why?
The purpose of a qualitative assessment of symptoms and needs in cancer settings is about:
- improving the quality of health care (targeting each patient’s needs and directing resources to optimize patient’s clinical outcomes);
- improving clinician–patient communication; and
- regularly monitoring physical, social and psychological functioning to better address these needs.
The qualitative assessment of symptoms and psychosocial needs is not only useful for the orientation towards adequate care interventions but also for the patients themselves, who increasingly express their interest of being involved in their supportive care pathway.
When?
Symptoms and needs must be assessed as early as possible and at every “step” of the cancer journey: diagnosis, treatment, rehabilitation, follow-up and end of life.
Who?
The qualitative assessment of symptoms and needs should apply to all cancer patients and survivors. Health care professionals should incorporate the detection of patient-reported outcomes in their routine clinical activity.
What?
Qualitative assessment of symptoms and needs should cover:
- physical aspects (functional assessment and symptom burden)
- social aspects (family, relational, employment issues)
- psychological aspects (emotional, spiritual, sexual)
- perceived barriers to care
- satisfaction with cancer care.
How to assess?
Tools and measures should be defined at a local level, but they should share common characteristics agreed at the European level. They should be:
- very brief;
- validated in the local language (patient’s language); and
- good performance parameters: validity, reliability, sensitivity, specificity, positive predictive value.
The literature emphasizes that tools should be accepted and shared by the front-line staff that will be using them in order to enhance the collaboration.
The qualitative assessment of symptoms and needs can be performed with traditional tools (paper and pencil tests) but also with the more recent digital tools, which have some limitations but also promising opportunities.
Personal interactions between health professionals and patients remain crucial to the process of obtaining valuable, reliable and viable information by which to initiate appropriate biomedical and/or psychosocial treatment.
Final objective
Every European cancer patient and survivor should have an assessment of symptoms and psychosocial needs that should be incorporated into the formal patient record system.